Claims Selection: Regenerate
Operation > Create Claims
A claim can only be Generated one time, either to ECS or paper (UB or CMS). For subsequent resubmission, claims must be Regenerated or Reprinted.
- To print or transmit additional claims, the Regenerate radio dial must be selected.
- Date of Service will default to the past 30 days but can be edited by manually entering a date or selecting from drop down calendar. Limit is 24 months.
- Criteria (ECS, UB, and or CMS) must be selected by checking the appropriate check box.
- In addition to selecting the date range, selections can be made by Payer and/or Patient.
The graphic below shows the Regenerate Claims option with 2 patients selected and the associated claims displayed.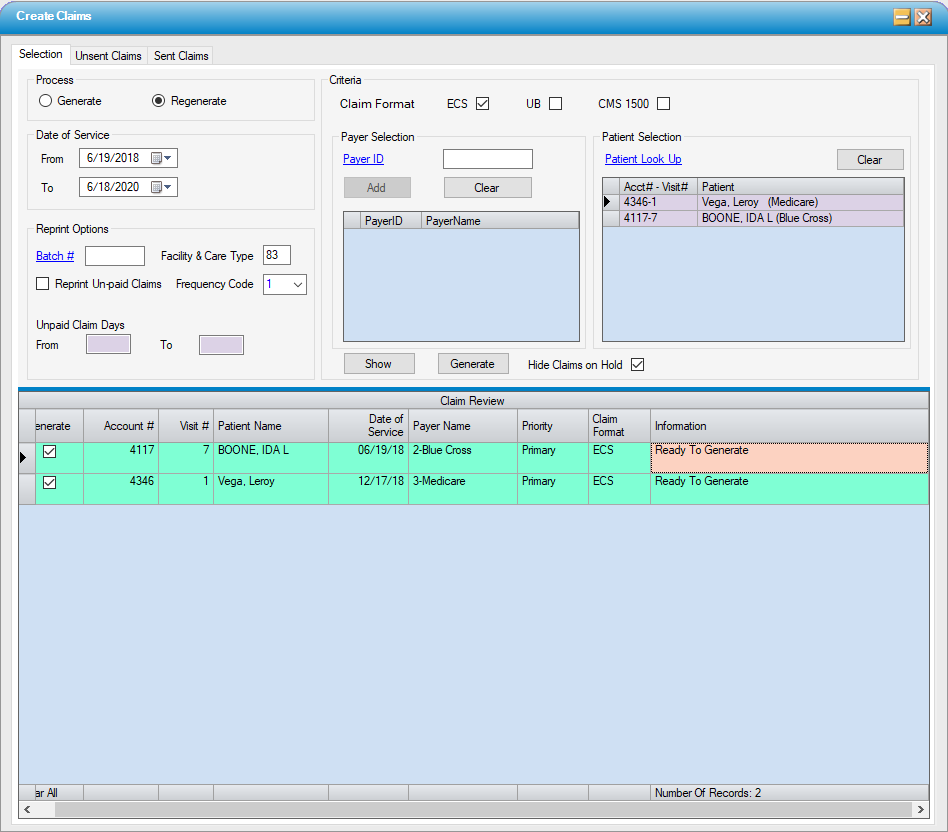
Regenerate claims
- Select Regenerate radio dial.
- Enter a date range in the Date of Service section; up to 24 months. (This field defaults to encompass a range of 30 days prior to the current date, so for recent claims, it may not be necessary to enter the date range.)
- Select a payer(s) or a patient(s):
- For Payer Selection, enter the Payer ID and select the Add function or use the hyperlink to search by Name, Address Line 1, Zip Code, or ECS Payer ID.
- For Patient Selection, use the Patient Look Up hyperlink to search by Last Name, First Name, Admit Date, or Account Number.
- Select
 and repeat for additional payers or patients. (Select
and repeat for additional payers or patients. (Select  to clear the selection grid and begin again.)
to clear the selection grid and begin again.)
- Select
 . The selected claims will display in the Claim Review grid.
. The selected claims will display in the Claim Review grid.
- Select
 to regenerate the claims.
to regenerate the claims.
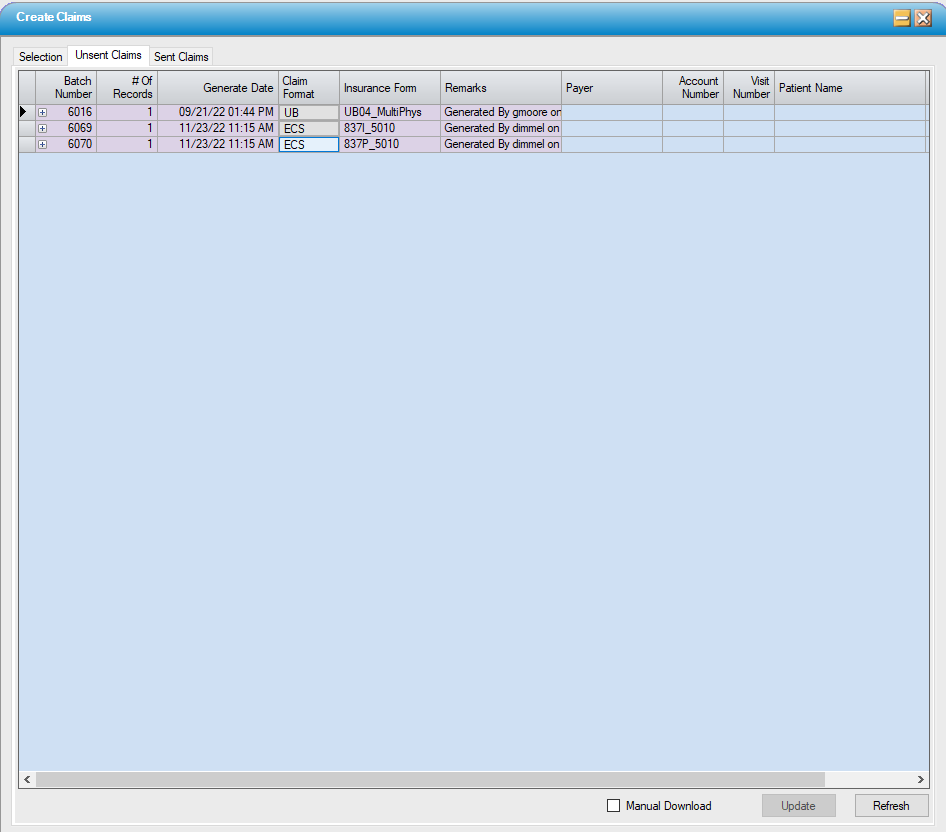
- Go to Unsent Claims to print and/or transmit the claims generated following the same steps utilized when Generating claims.
Reprint Options
- The Regenerate radio dial must be selected to utilize Reprint Options.
- To reprint an entire batch, use the Batch # hyperlink to search by Date or Batch #.
- To reprint for a specific payer(s) or patient(s), follow the instructions above for Payer and Patient Selection.
- Facility & Care Type will default to the Facility & Care Type selected in Center Configuration > Misc tab but can be edited here if the center has experienced transitions in the type of care provided (such as temporarily participating in the Hospitals Without Walls program).
- Frequency Code indicates whether the claim is new, a replacement (corrected) claim, or a claim to be voided. This, in conjunction with the Facility & Care Type, is the number that populates in box 4 of the UB04 claim form to. Select from:
- 1 - Original (default)
- 7 - Replacement
- 8 - Void
NOTE: For Corrected Claims that require the original claim number appear on the corrected claim, complete the ICN field on the Billed Payers tab of the Patient Account. (This field will populate automatically if payment and/or denial was entered via Electronic Remittance Advice - Payer.)
- Reprint Unpaid Claims will regenerate claims for all previously generated claims for which no payment has been posted up to aging of 365 days. This function can be utilized for resubmission of unpaid claims or for working those unpaid claims.